Labiaplasty & Gynecologic-Oncologic Reconstruction in Newport Beach, CA.
Labiaplasty
Labiaplasty is one of the more common flaps used in vulvar reconstruction. And, when there is a cancer located on the vulva, the contralateral non-affected side will undergo a labiaplasty for symmetry.
Labiaplasty as a purely cosmetic operation is usually performed in conjunction with another cosmetic procedure. For example, a female patient in her 40’s who is undergoing removal of her mammary prosthesis and breast lift can undergo labiaplasty at the same time under the same general anesthetic. The labiaplasty takes approximately 1 hour. The suture line is placed on the posterior aspect of the vagina and not anteriorly to facilitate healing and prevent pain with sexual intercourse. The sutures used for labiaplasty are absorbable. That means, there are no sutures to take out after surgery. We encourage you to shower on post-operative day two and wash the surgical areal with soap and water. At night it is important not to wear any constrictive clothing such as spanks that might keep moisture in the perineum and groin. Sleeping in a night gown and having the surgical site air out is best for healing. Antibiotics are prescribed for one week postoperatively and patients are on pain pills for about 2-3 days postoperatively. It is ok to return to baths or swimming after the six-week mark. Patient satisfaction is quite high after labiaplasty.
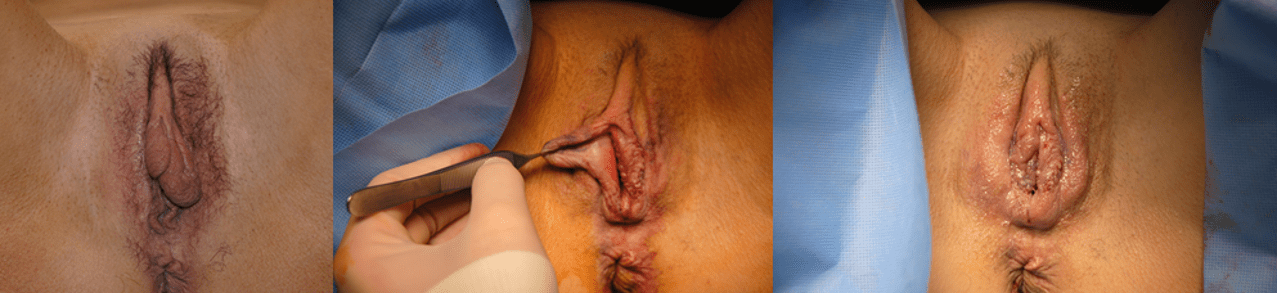 Bilateral Labiaplasty and Vulvar Cancer Resection
Bilateral Labiaplasty and Vulvar Cancer Resection
Gynecologic-Oncologic Reconstruction
Gynecologic-Oncologic Reconstruction is another challenging aspect of Plastic & Reconstructive surgery. As in breast cancer treatment and reconstruction, a gynecologic cancer diagnosis can be emotional and confusing. It is important to keep things simple. The principles are to restore the anatomy to the best of what your local tissues will allow us to do. If the local tissue is unable to close the defect that resulted from your cancer, then we use regional or distant tissue to help close the defect. We plan our closures in a manner that can get you on to radiation therapy or chemotherapy in a timely manner as often these modalities are just as important if not more important than surgery.
Vulvar Cancer
Vulvar cancer is a cancer of the female labia. In general, the surgical excision and the reconstructive surgery is performed at the same time with the gynecologic-oncologic surgeon and the plastic & reconstructive surgeon. Often the reconstruction involves using the redundant labia and when necessary, the medial thigh skin to help close any defects. It is important to eat a diet high in protein for 4-6 weeks prior to surgery and for 4-6 weeks after surgery. It is quite common for recurrent vulvar cancers to present themselves and often this area has been previously radiated. In patients who have previously undergone radiation therapy we recommend 2-3 treatments of hyperbaric oxygen prior to surgery and 2-3 treatments after surgery. It is ok to shower two days after surgery and it is important to keep the groin and perineum clean and dry following surgery. We try to avoid any creams or ointment in this area as it can often macerate the skin.
To read more about Vulvar Cancer, please click on the following link: https://medcraveonline.com/OGIJ/OGIJ-12-00607.pdf
Vaginal Cancer
Vaginal cancers are located on the inside of the vagina and for reconstructive purposes classified as in the proximal or distal aspect of the vagina. For cancers that are on the distal or most outward part of the vagina the defect after resection can be reconstructed with skin from the medial aspect of the inner thigh. Previous radiation to the groin can make this reconstruction more challenging, but still very possible. It is important prior to vaginal reconstruction to have a diet high in protein. You should aim to consume about 1.5 grams of protein per kilogram of body weight. Hyperbaric oxygen therapy is an important adjunct prior to and after surgery to facilitate wound healing. When the flap from the groin is rotated into the vagina, the medial thigh skin can often become macerated. It is important to keep the groin area clean and dry to facilitate healing and prevent wound breakdown. I try to reiterate with patients that the incidence of wound dehiscence or wound breakdown is quite high with vaginal reconstruction simply because it is a tough area to heal, and previous radiation therapy is likely. We have a low threshold for returning to the operating room to close any wound dehiscence you may have. It is important to close these wounds prior to radiation therapy and/or chemotherapy.
Vaginal cancers of the proximal vagina will usually require a myocutaneous flap such as a gracilis flap from the medial thigh to close the defect. The gracilis myocutaneous flap has a longer reach and can extend to cover the entire length of the vaginal canal. In cases where the entire vaginal canal needs to be reconstructed, bilateral gracilis myocutaneous flaps can be used to reconstruct the entire vaginal canal.
To read more about Vaginal cancer reconstruction, please click on the following link: https://medcraveonline.com/OGIJ/OGIJ-12-00607.pdf
Gynecological cancers and Pelvic Exenteration:
In cases of uterine or cervical cancer that extend to other organs in the pelvis such as the bladder, rectum, and pelvic side walls, a pelvic exenteration is performed. In this operation the uterus, ovaries, and possibly some combination of rectum and bladder is removed from the pelvis. In these cases, the fecal and urinary streams are often diverted and joined together or separately. In these cases, the vertical rectus abdominus myocutaneous flaps is utilized to reconstruct the pelvis. The bulk of the VRAM can be utilized to obliterate the “dead space” in the pelvis to prevent the bowel from adhering to the denuded pelvis. The VRAM flap can also be utilized to reconstruct the vaginal canal and can serve as a pedestal for ureteral conduit reconstruction. This can prevent post-operative seroma formation and infection and prevent leak from the urinary system.
It is important for patients to consume a diet high in protein for 4-6 weeks before surgery and then as soon as bowel function returns after surgery. The metabolic demands of recovering from this surgery is high and protein intake needs to be maximized prior to surgery.
To read more about Gynecological cancers and Pelvic Exenteration, please click on the following link: https://medcraveonline.com/OGIJ/OGIJ-12-00607.pdf
If you have a gynecological cancer and need reconstruction, you will be referred by your gynecologic oncologist to our practice. We look forward to working with you.
